Infection by T. gondii can lead to toxoplasmosis, and can be transmitted to humans by animals, cats in particular, posing a special danger to pregnant women, and unborn infants.
The good news is that most studies show that contact with a pet cat or a neighbor’s cat will not increase the risk of acquiring toxoplasmosis, unless these animals are allowed to roam and hunt or eat raw meat. However, contact with stray and feral cats can be risky.
Domestic, wild, and feral cats frequently transmit Toxoplasma infection to humans, through a process generally known as zoonosis.
Be advised then that to some extent symptoms listed may indicate the presence of the T. gondii parasite in pets and other animals.
Though figures vary greatly, As much as 50% of the human population in general, 11-23% in the United States and 20% to 80% of all domestic animals are infected with Toxoplasma, harboring its cyst form.
If given the opportunity, the cyst can produce chronic, severe, possibly fatal symptoms in immunocompromised and special risk patients, pregnant mothers and even their unborn child.
History
The protozoan was first discovered by Nicolle & Manceaux, who in 1908 isolated it from the African rodent Ctenodactylus gundi, then in 1909 differentiated the disease from Leishmania and named it Toxoplasmosis gondii.
The first recorded congenital case was not until 1923, and the first adult case not until 1940.
In 1948, a serological dye test was created by Sabin & Feldman, which is now the standard basis for diagnostic tests.
Just Not Feeling It?
Like many other infectious agents symptoms can be generalized and ill-defined.
Infection is common, but full-blown disease is rare.
Such tactics are very much the way many organisms, parasites in particular, are able to succeed and persist in nature.
Symptoms may take weeks or months to manifest, in part or on the whole, and may eventually subside on their own without ever being specifically recognized or clinically tested and diagnosed.
Clearly this emphasizes why it is important advice to see a doctor regularly and right away when experiencing any unusual issues.
Clinical manifestations
Infection has two stages:
Acute toxoplasmosis
During acute toxoplasmosis, symptoms are often influenza-like: swollen lymph nodes, or muscle aches and pains that last for a month or more.
Rarely, a patient with a fully functioning immune system may develop eye damage from toxoplasmosis.
This can sometimes cause damage to the brain or the eyes.
Latent toxoplasmosis
Most patients who become infected with Toxoplasma gondii and develop toxoplasmosis do not know it.
In most immunocompetent patients, the infection enters a latent phase, during which only bradyzoites are present, forming cysts in nervous and muscle tissue.
Most infants who are infected while in the womb have no symptoms at birth but may develop symptoms later in life.
Only a small percentage of infected newborn babies have serious eye or brain damage at birth.
Special Risk Factors
Young children, patients being treated for cancer taking certain types of chemotherapy, those who have recently received an organ transplant or with AIDS may experience more severe symptoms and complications from toxoplasmosis infection.
Mortality rates can be particularly high for these affected individuals.

Diagnosis
Seek a clinical doctor or a veterinarian as is appropriate to the particular patient involved.
Blood serology tests may indicate recent infection with T. gondii, but not a definitive diagnosis of toxoplasmosis.
Diagnosis relies on the history of the patient, symptoms, and the results of laboratory tests, including an antibody titer test and microscopic examination of tissues.
If a healthy cat has high antibody levels, that means it has been previously infected and is now probably immune and not excreting oocysts to other animals.
If there is no antibody, the cat is able to become infected in which case it would shed oocysts for one to two weeks after exposure.
Mainfestations of T. gondii
Toxoplasmosis Acute Symptoms:
- Mild Flu-like symptoms
- Swollen Lymph Nodes
- Muscle Aches and Pains
- Lethargy
- Fever
- Vomiting
- Diarrhea
- Cysts
Latent or Severe Symptoms:
- Difficulty in chewing and swallowing food
- Loss of appetite
- Weight Loss
- Anorexia
- Personality changes
- Depression
- Circling
- Difficulty Breathing (because of pneumonia)
- Eye Inflammation
- Abnormal-sized pupils
- Inflammation of the Retina
- Blindness
- Inflamed pancreas
- Enlarged lymph nodes
- Liver inflammation
- Jaundice
- Neurological Symptoms
- Ear twitching
- Lack of coordination
- Seizures
- Loss of control over urination and defecation
Other Manifestations?
Read: “What the Cat Dragged In…” for more detailed information on how the parasite T. gondii is supposed to influence a host’s behavior beyond the indications and symptoms listed here.
Variations?
Read: “What is Zoonosis” For more detailed information on other types and background on Animal Disease transmission.
Why Blame the Cat?
Cats are the only known definitive hosts in which the parasite may undergo sexual reproduction to complete their life cycle. Cats have a 20% to 60% infection rate with T. gondii.
Toxoplasmosis is most common in cats less than two years old, possibly because of their poorly developed immune response or diet.
Stray and feral cats have a higher incidence of infection than pet cats. Toxoplasmosis occurs more frequently in kittens, young adult, and very old cats have a greater chance of acquiring it.
In an older cat, a recurrent infection may be due to the presence of feline leukemia virus or feline immunodeficiency virus, which suppress its immune response.
Such prevalence is related to certain factors including the ingestion of infected animals such as rodents and birds or raw meat.
However, most often cats will demonstrate virtually no observable symptoms of an infection by Toxoplasma, so by all means be vigilant when handling cats and their overall maintenance.
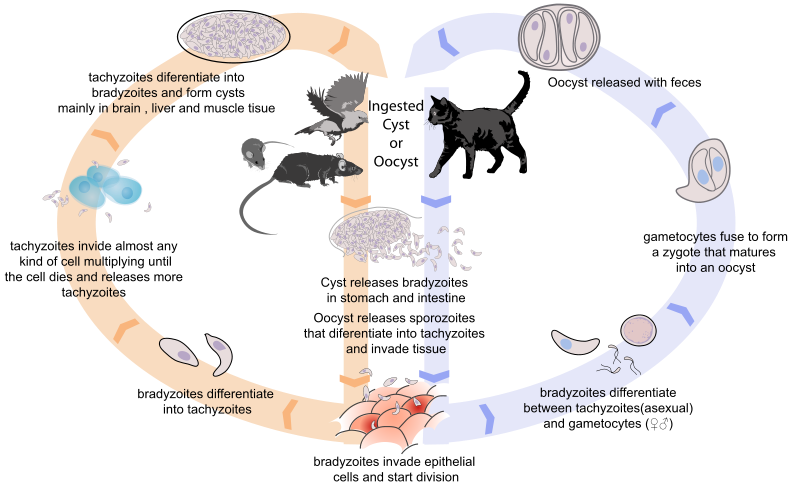
Life Cycles of T. gondii
T. Gondii has 3 life stages
Oocysts have 2 reproductive methods:
Sexual reproduction
Only occurs in cats (Definitive Host)
- Cyst, (oocyst, or tachyzoite). A cat may eat cysts containing bradyzoites in infected rodents or birds, or other raw meat, whereupon the organisms will begin to multiply in the wall of the small intestine epithelium where they turn into merozoites and convert into the noninfectious sexual stages of the parasite to undergo sexual reproduction, producing the second life stage; zygote-containing oocysts.
- Feline shedding of oocysts
Studies have shown that only about 2% of cats are shedding oocysts at any one time. Although the pathogen has been detected on the fur of cats, it has not been found in an infectious form, and direct infection from handling cats is generally believed to be very rare.Oocyst shedding does not recur even after repeated exposure to the parasite.
Most exposed cats spred oocysts during acute Toxoplasma infection, but not after. Cats excrete the pathogen in their faeces for two to three weeks after contracting the disease. Oocysts are very hardy and can survive in moist shaded soil or sand for months.
Even then, cat faeces are not generally contagious for the first day or two after excretion, after which the cyst ‘ripens’ and then they may become spores becoming potentially pathogenic sporozoites.
Asexual reproduction
Any warm-blooded animal (Intermediate Host)
- Spores (sporozoites) become infectious to other animals, including humans. In the intestine, some Toxoplasma organisms multiply in a stage of rapid division as tachyzoites, which spread to other sites in the body. This stage eventually ends.
- Tissue Cysts (bradyzoite) A "resting" stage of slow division produces cysts in the muscles and brain. Most of these cysts probably remain dormant indefinitely.

T. gondii transmission may occur through:
- Ingestion of raw or partly cooked meat, especially pork, lamb, or venison containing Toxoplasma cysts. Infection prevalence in countries where undercooked meat is traditionally eaten, such as France, has been related to this transmission method. Oocysts may also be ingested during hand-to-mouth contact after handling undercooked meat, or from using knives, utensils, or cutting boards contaminated by raw meat.
- Ingestion of contaminated cat faeces.
- Hand-to-mouth contact after touching anything that has come into contact with cat faeces.
- Water contaminated with Toxoplasma.
- Infected organ transplant or blood transfusion, although this is extremely rare.
Oocysts may exist in:
- Cutting Boards
- Unwashed Vegetables
- raw or partly cooked meat
- Garden soil
- Children’s sandboxes
- Litter boxes
- Anything that has come into contact with cat faeces
Help control the spread of Toxoplasma!
Restrict your pet cats from access to rodents and birds, and give them only cooked meat, commercially prepared cat food, and pasteurized dairy products. Don’t allow them to scavenge in garbage cans.
Avoid Oocyst Transmission:
- Wear rubber gloves during contact with contaminated soil or litter.
- Wash hands thoroughly after contact.
- Cover sandboxes to prevent cats from defecating in them.
- Get rid of feces from litter boxes every day
- Disinfect with scalding hot water and/or dry heat
Chemical disinfectants will not effectively destroy T. gondii oocysts!
The cyst form of the parasite is extremely hardy, capable of surviving exposure to freezing down to −12 degrees Celsius (10 degrees Fahrenheit), moderate temperatures and chemical disinfectants such as bleach, and can survive in the environment for over a year. It is, however, susceptible to high temperatures—above 66 degrees Celsius (150 degrees Fahrenheit), and is thus killed by thorough cooking, and would be killed by 24 hours in a typical domestic freezer.
Pregnancy Risk
Congenital toxoplasmosis is a special form in which an unborn child is infected via the placenta. A positive antibody titer indicates previous exposure and immunity and largely ensures the unborn baby’s safety.
A simple blood draw at the first pre-natal doctor visit can determine whether or not the woman has had previous exposure and therefore whether or not she is at risk. If a woman receives her first exposure to toxoplasmosis while pregnant, the baby is at particular risk. A woman with no previous exposure should avoid handling raw meat, exposure to cat feces, and gardening (cat feces are common in garden soil).
Most cats are not actively shedding oocysts and so are not a danger, but the risk may be reduced further by having the litterbox emptied daily (oocysts require longer than a single day to become infective), and by having someone else empty the litterbox.
However, while risks can be minimized, they cannot be eliminated.
For pregnant women with negative antibody titer, indicating no previous exposure to T. gondii, as frequent as monthly serology testing is advisable as treatment during pregnancy for those women exposed to T. gondii for the first time decreases dramatically the risk of passing the parasite to the fetus.
But the greatest concern for humans is transmission of Toxoplasma from mother to fetus.
Up to 45% of American women between the ages of 20 and 39 have already been exposed to Toxoplasma and are therefore immune. But in mothers who first acquire Toxoplasma infection during their pregnancy, about one-third to one-half of their infants born to mothers are also infected.
Toxoplasma infection of the fetus is least common, but the disease is most severe, if the mother has been infected during the first trimester of pregnancy.
Toxoplasma infection is most common, but the disease is least severe or without symptoms, if the infection occurs during the third trimester.
Most women infected during pregnancy have no symptoms of the infection themselves, but there is about a 40% chance that the fetus will acquire the infection, and be born prematurely or even stillborn. In about 10% of these cases, severe neurological or eye disease will result.
Toxoplasma infection results in over three thousand human congenital infections annually in the United States, most of them with no symptoms. In symptomatic individuals, symptoms may appear at different times: at birth, or weeks, months, or even years later.
Pregnancy precautions:
If you are pregnant, or plan to become pregnant soon:
- Test your cats for antibodies to Toxoplasma
- Do not allow cats access to birds, rodents
- Avoid contact with uncooked meat, and unpasteurized dairy products
- Wash uncooked vegetables thoroughly before eating
- Don’t handle litter boxes; have another person change them daily
- Wash hands thoroughly with soap and water after contact with soil and cats.
- Stay away from free-roaming cats because they can be contaminated with oocysts.
- Keep any outdoor cat from contact with bedclothes and any furnishings that you use.
- Don’t handle a cat that seems ill.
Despite these risks, pregnant women are not routinely screened for toxoplasmosis in most countries (France, Austria and Italy being the exceptions) for reasons of cost-effectiveness and the high number of false positives generated as the disease is so rare (an example of Bayesian statistics).
As invasive prenatal testing incurs some risk to the fetus (18.5 pregnancy losses per toxoplasmosis case prevented), postnatal or neonatal screening is preferred. The exceptions are cases where foetal abnormalities are noted, and thus screening can be targeted.
Some regional screening programmes operate in Germany, Switzerland and Belgium.
Treatment is very important for recently infected pregnant women, to prevent infection of the fetus. Since a baby’s immune system does not develop fully for the first year of life, and the resilient cysts that form throughout the body are very difficult to eradicate with anti-protozoans, an infection can be very serious in the young.
Transplacental transmission:
(a) Infection in 1st trimester – incidence of transplacental infection is low (15%) but disease in neonate is most severe.
(b) Infection in 3rd trimester – incidence of transplacental infection is high (65%) but infant is usually asymptomatic at birth.
Toxoplasmosis Treatment
No vaccine is currently available.
Treatment is often only recommended for people with serious health problems, because the disease is most serious when one’s immune system is weak.
Pyrimethamine and Sulfadiazine are the two drugs used to treat toxoplasmosis.
They act together to inhibit Toxoplasma reproduction. However, pyrimethamine may be unpalatable or even toxic to some cats.
Another choice is the antibiotic clindamycin, which has fewer side effects. Alternative veterinarians recommend modalities such as herbs, homeopathy, and acupuncture to treat the symptoms of toxoplasmosis.
Medications frequently prescribed for Acute Toxoplasmosis are:
- Pyrimethamine An anti-malarial medication.
- Sulfadiazine Antibiotic used in combination with pyrimethamine to treat toxoplasmosis.
- Clindamycin Antibiotic used most often for people with HIV/AIDS.
- Spiramycin Antibiotic used most often for pregnant women to prevent the infection of their child.
(Other antibiotics such as minocycline have seen some use as a salvage therapy).
In people with latent toxoplasmosis, the cysts are immune to these treatments, as the antibiotics do not reach the bradyzoites in sufficient concentration.
Medications prescribed for Latent Toxoplasmosis are:
- Atovaquone — an antibiotic that has been used to kill Toxoplasma cysts inside AIDS patients.
- Clindamycin — an antibiotic which, in combination with atovaquone, seemed to optimally kill cysts in mice.
However, in latent infections successful treatment is not guaranteed, and some subspecies exhibit resistance.
Sources:
Centers for Disease Control
Supplemented by: Wikipedia Toxoplasma gondii
and Other Non-Specific Sources